Understanding the Intersection of Diabetes and Psychiatric Disorders
When considering the complex tapestry that is human health, few intersections are as intricate and profound as that between type 2 diabetes (T2D) and psychiatric disorders. Delving into this interplay reveals not only a prevalence of mental health issues amongst those living with T2D but also the myriad of ways in which these conditions can complicate each other.
Exploring the Prevalence of Psychiatric Disorders Among Individuals with Type 2 Diabetes
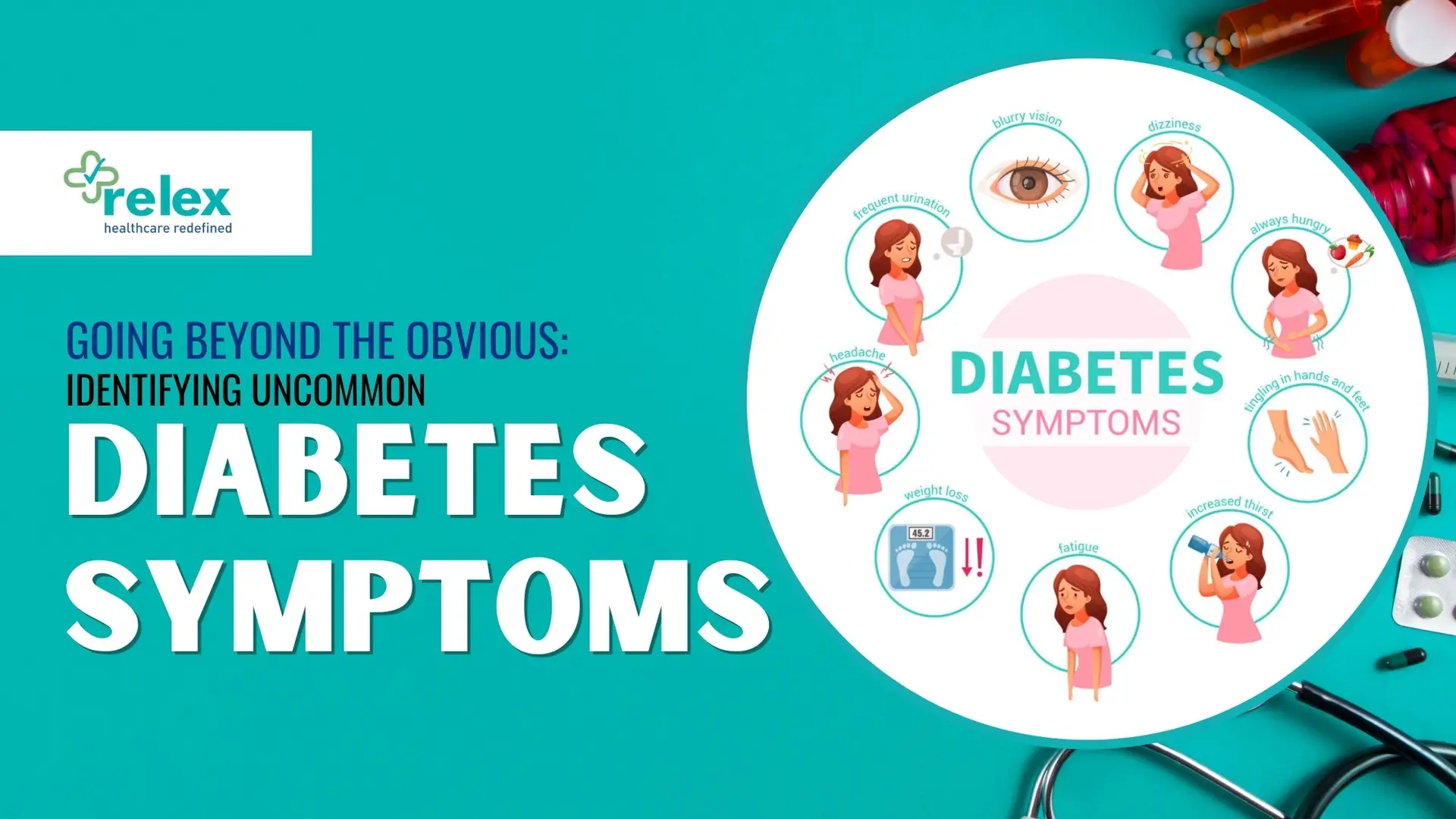
The relationship between type 2 diabetes and psychiatric disorders is bidirectional and fraught with complications. Studies have shown that individuals with schizophrenia, for instance, may have impaired glucose tolerance rates as high as 30%, depending on factors like age, genetics, and environmental conditions [PubMed]. The connection doesn’t end there—sleep disorders, binge eating, substance use, and anxiety disorders have all been linked with increased instances of type 2 diabetes, painting a picture of a pervasive and troubling trend [PubMed]. Psychiatric medications themselves often contribute to this problem by inducing weight gain and complicating blood sugar management, further entwining these health challenges.
Impact of Psychological, Cognitive, and Emotional Issues on Diabetes Management
The presence of psychiatric disorders can significantly hinder the effective management of diabetes. Mood fluctuations, cognitive impairments, and other psychological barriers make consistent self-care more challenging. A patient’s ability to maintain a healthy diet, monitor blood glucose levels, and adhere to medication regimens can be severely disrupted by underlying mental health issues. In essence, the psychological state of an individual with T2D is as crucial as their physical state when it comes to managing the disease effectively.
Challenges Faced by Individuals with Comorbid Diabetes and Psychiatric Illness in Receiving Adequate Care
The convergence of T2D with psychiatric conditions presents a complex challenge for healthcare delivery. The comorbid nature of these illnesses often leads to disparities in care, as traditional healthcare systems may not be equipped to address both sets of needs simultaneously. Moreover, social stigma surrounding psychiatric disorders can prevent patients from seeking the care they need, thereby exacerbating their overall condition. The integration of care for such dual diagnoses is paramount, yet it remains an area of ongoing concern and development within the medical community.
In order to effectively confront these issues, a multifaceted approach that considers the uniqueness of each individual’s situation is essential. Healthcare providers must navigate these troubled waters with sensitivity and a comprehensive understanding of how these health issues intersect and influence one another. From tailored treatment plans to vigilant monitoring of both physical and mental health symptoms, the care for individuals grappling with both T2D and psychiatric disorders demands attention, compassion, and innovation.
Importance of Treatment Adherence in Dual Diagnosis Cases
In the realm of chronic conditions like type 2 diabetes, adherence to treatment is pivotal. But what happens when another layer—psychiatric illness—is added to the mix? The significance of following medical advice becomes even more crucial, as it’s a linchpin in managing both conditions effectively.
Significance of Treatment Adherence in Managing Diabetes and Psychiatric Disorders
Imagine two gears in a machine that need to work in tandem for smooth operation. In a similar fashion, managing type 2 diabetes demands a strict regimen of medication, diet, and exercise, while psychiatric disorders call for consistent therapy and pharmacological interventions. When these gears are synchronized through treatment adherence, patients are more likely to maintain glycemic control, reducing the risk of complications and improving overall prognosis. Notably, this coordination is also cost-effective by diminishing hospitalizations and other healthcare expenses associated with complications from poorly managed diabetes (Psychosocial Determinants of Treatment Adherence in Patients with Type 2 Diabetes – A Review).
Factors Influencing Poor Treatment Adherence in Individuals with Comorbid Conditions
Poor treatment adherence in individuals with dual diagnoses can stem from a complex web of factors. For one, the presence of psychological symptoms such as depression or anxiety can sap motivation and energy, making it difficult for patients to keep up with their treatment plans. Additionally, cognitive impairments or stress may lead to forgetfulness or intentional skipping of medication doses (Psychosocial Determinants of Treatment Adherence in Patients with Type 2 Diabetes – A Review). Financial constraints, lack of social support, or simply the overwhelming nature of managing multiple health issues simultaneously can also contribute to non-adherence.
Role of Self-Management in Effective Diabetes Care for Patients with Psychiatric Illnesses
When we talk about self-management in diabetes care, especially for those grappling with psychiatric illnesses, we’re honing in on empowering patients with the knowledge, skills, and confidence to take control of their own health. This includes understanding their conditions, knowing how to monitor blood glucose levels, recognizing the signs of hypo- or hyperglycemia, and being aware of how to respond accordingly. Self-efficacy plays a pivotal role, as it’s linked with better medication adherence and, consequently, improved quality of life (Psychosocial Determinants of Treatment Adherence in Patients with Type 2 Diabetes – A Review). By fostering a sense of autonomy and competence, patients can navigate the complexities of their dual diagnosis with greater ease.
Strategies for Enhancing Treatment Adherence and Self-Management
Improving treatment adherence in individuals with type 2 diabetes who are also managing psychiatric disorders can seem daunting. Nevertheless, a multifaceted strategy that includes optimizing healthcare utilization, employing psychological approaches, and involving patients and caregivers in the decision-making process holds promise for better outcomes.
Utilizing Healthcare Utilization for Improving Treatment Adherence in Dual Diagnosis Cases
Healthcare professionals play an instrumental role in fostering treatment adherence through personalized diabetes self-management education and support (DSMES). By providing patients with the necessary knowledge and skills, DSMES empowers them to make informed decisions about their self-care. This educational approach is critical for dual diagnosis cases where the complexity of managing both diabetes and a psychiatric disorder requires a higher level of understanding and engagement from the patient. Evidence suggests that improved health literacy is a key predictor of diabetes treatment adherence, highlighting the need for clear communication and accessible information for patients.
Psychological Approaches to Enhance Therapeutic Adherence in Diabetes Care
Mental well-being is as crucial as physical health in managing diabetes effectively. Mental health specialists can guide patients through the emotional aspects of their condition, helping to lighten the mental load that often accompanies chronic illness management. A qualitative study pointed out that the support umbrella, which encompasses emotional, informational, and practical support, is vital for encouraging treatment adherence. Psychological interventions, like Cognitive Behavioral Therapy (CBT) and motivational interviewing, have been shown to improve therapeutic adherence by addressing the underlying beliefs and behaviors that impede self-care practices.
Involving Patients and Caregivers in Decision-Making Processes for Comprehensive Management
Shared decision-making is a cornerstone of comprehensive diabetes management, particularly when patients are also dealing with psychiatric issues. Involving patients and their caregivers in the care plan not only bolsters treatment adherence but also enhances the patient’s sense of control and satisfaction with their treatment. The qualitative study mentioned earlier emphasizes the theme of ‘responsibility’, indicating that when patients feel accountable for their health outcomes, they are more likely to adhere to their treatment regimen. This sense of ownership, combined with the support from healthcare providers, encourages a more active role in disease management.
By integrating these strategies—leveraging healthcare education, psychological support, and active patient involvement—patients with comorbid diabetes and psychiatric disorders can achieve better self-management and adherence to treatment. These efforts not only improve individual health outcomes but also contribute to the overall effectiveness and efficiency of healthcare delivery.
Collaborative Care Approaches for Diabetes and Psychiatric Disorders
In the journey of managing type 2 diabetes coupled with mental health challenges, the pathway to wellness is not a solitary trek, but rather a team expedition. Recognizing patients and caregivers as crucial stakeholders in this journey is pivotal. They are the compass and map holders, guiding treatment directions based on the landscape of their unique experiences and needs.
Recognizing patients and caregivers as crucial stakeholders in the management plan
Living with type 2 diabetes demands constant vigilance; when psychiatric disorders enter the mix, the complexity intensifies. Patients and caregivers, who engage daily with these conditions, hold invaluable insights into the nuances of care that can often go unnoticed in clinical settings. Their contributions to the management plan are essential, providing context and real-life feedback that can enhance the effectiveness of treatment strategies. As partners in care, they help bridge the gap between medical recommendations and day-to-day implementation, ensuring that care plans are not only clinically sound but also practically feasible.
Encouraging shared decision-making to empower patients in their care
The road to empowerment in healthcare is paved with shared decision-making. When patients are active participants in their treatment choices, they often experience a greater sense of control and satisfaction with their care. This collaborative approach is especially significant for those juggling the demands of diabetes and mental health issues. Shared decision-making fosters a deeper understanding and commitment to the chosen treatment, which can lead to improved outcomes. It’s about crafting a care plan in tandem with healthcare professionals—one that resonates with the patient’s values, preferences, and lifestyle.
Emphasizing the need for interdisciplinary collaboration between endocrinologists and psychiatrists
The confluence of diabetes and psychiatric disorders calls for an orchestra of expertise, harmonizing the skills of endocrinologists with psychiatrists. This interdisciplinary collaboration creates a holistic approach to patient care that addresses both the physical and psychological aspects of these comorbid conditions. Endocrinologists provide the framework for managing blood sugar levels and other metabolic concerns, while psychiatrists tend to the emotional and cognitive well-being of patients. Together, they can tailor a more comprehensive and responsive treatment regimen that acknowledges the interplay between mind and body.
Such integrated care models have been shown to be effective. A systematic review and meta-analysis highlighted that collaborative care models can improve depression outcomes and quality of life for patients with comorbid depression and diabetes (Wang et al., 2022). By drawing upon the strengths of each discipline, the collaborative approach aims to enhance the overall health and well-being of individuals facing the dual challenges of diabetes and psychiatric illness.
As we’ve explored previously, the significance of treatment adherence in managing diabetes and psychiatric disorders cannot be overstated. The collaborative care model dovetails nicely with this concept, as it inherently promotes adherence through its patient-centered focus and multi-disciplinary support system. By involving both patients and caregivers in the decision-making process, collaborative care reinforces the importance of personalized education and emotional support, furthering the goals set forth in enhancing treatment adherence and self-management.
In closing, it’s important to reflect on the collective efforts that make managing such complex health conditions possible. The collaborative care approach in diabetes and psychiatric disorders exemplifies the power of unity in healthcare—where patients, caregivers, and a diverse team of healthcare professionals come together to navigate the emotional rollercoaster with wisdom, compassion, and shared purpose.
Future Directions and Implications for Healthcare Professionals
The multifaceted nature of the interaction between diabetes and psychiatric disorders presents intricate challenges and opportunities for healthcare professionals. As we look toward future directions in treatment and care, it’s clear that an increased understanding of these complexities is crucial for effective management of dual diagnosis cases. But what does this entail, and how can healthcare providers enhance their approach to benefit individuals with comorbid conditions?
Multifaceted Nature of the Interaction Between Diabetes and Psychiatric Disorders
Firstly, it is important to recognize that the relationship between diabetes and psychiatric disorders is bidirectional; each condition can exacerbate the other. For instance, diabetes can lead to psychological distress due to its chronic nature, while psychiatric disorders can complicate diabetes management via poor lifestyle choices or medication nonadherence. This interplay necessitates a holistic approach in patient care, where physical and mental health are treated concurrently. Future healthcare strategies must integrate more robust screening and monitoring systems that account for both sets of conditions.
Importance of Increased Understanding for Effective Management of Dual Diagnosis Cases
An in-depth understanding of how psychiatric disorders intersect with diabetes is imperative for healthcare professionals. Training programs should incorporate modules on the psychological aspects of diabetes management, highlighting the importance of mental well-being in achieving optimal glycemic control. This education should extend to recognizing signs of mental distress and the potential impact on diabetes care. Professionals must be adept at identifying symptoms that may indicate a need for psychiatric intervention, which could range from psychotherapy to pharmacological treatments.
Opportunities for Healthcare Professionals to Enhance Care Delivery for Individuals with Comorbid Conditions
The healthcare system has numerous opportunities to improve outcomes for patients with comorbid diabetes and psychiatric disorders. One avenue is the development of integrated care models that bring together endocrinologists, psychiatrists, psychologists, and primary care providers. Such collaboration ensures that all aspects of a patient’s health are addressed. Additionally, embracing technologies like telemedicine can provide ongoing support and monitoring, particularly for those in remote or underserved areas.
Healthcare professionals can also advocate for policies that support comprehensive care and push for research into new treatment modalities. There is hope on the horizon with advancements like cell therapy for diabetes, which aims to replace missing insulin-producing cells, potentially leading to a cure. Meanwhile, an emphasis on preventive measures, such as identifying at-risk individuals and implementing early intervention strategies, is also gaining traction. These efforts contribute to a paradigm shift from merely managing glucose levels to a more inclusive approach that also prioritizes weight management and cardiovascular health.
To mitigate the long-term effects of diabetes, such as damage to blood vessels and organs, healthcare professionals must be proactive in their approach, ensuring that both diabetic and psychiatric conditions are managed effectively. With a more comprehensive understanding of these interactions, they can deliver personalized care that addresses the unique needs of each patient. Encouraging adherence to treatment plans through patient education and engagement remains a cornerstone of successful management strategies.